New years eve, my good friend asked me what were the best things to happen to me this year? I answered, am.. I think… am…it has been a good year but I just cant think. Therapy was good.
Next day, my good friend asks me, what things make you happy? I answered, am.. I dunno, like loads of things, movies, music, my nieces….there’s more I just cant think.
A few months ago, I told someone that I could never understand how people were so self aware. How people could say things like. Every September I get my asthma really bad, its the change in the weather. People being able to pinpoint really specific events and how they felt made me hugely uncomfortable with myself, because I couldn’t do the same.
I am currently doing a mindfulness course. An eight week program by Williams and Penman. I have reached week six and have had a WOW moment. I found out why I cant recall specific memories. My memory of any of my hospitalisations are very vague but I sort of understood that, presumed I had repressed them as they were too bad. But I also thought that I was the least self aware person on the planet, because I have such difficulty recalling specifics. Turns out I have an over general memory.

Many theorists have suggested that the reduced ability to access specific memories of life events, termed overgenerality, is a protective mechanism helping attenuate painful emotions associated with trauma.
Mark Williams, PhD, a clinical psychologist and researcher at Oxford University, came across this term in the 1980’s when asking people to recall certain memories and they gave him vague responses. He had asked research subjects to write down the memories elicited by certain cues. After investigators read them a cue word, they have 30 seconds to recount a single specific memory, meaning an event that lasted less than one day. When they left the page blank he thought he had given unclear instructions. Soon he began to wonder about the significance of the omissions.
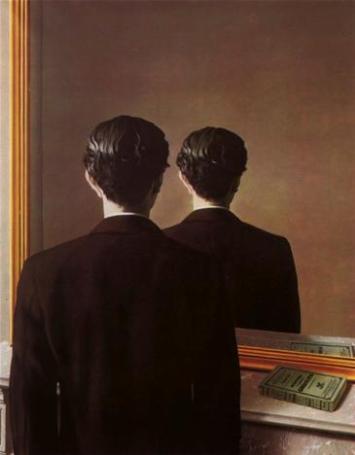
Usually people seeking a particular memory traverse a mental hierarchy, Dr. Williams said. They begin by focusing on a general description (“playing ball with my brother”) and then narrow the search to a specific event (“last Thanksgiving”). Some people stop searching at the level of generality, however and are probably not conscious of having done so.
In response to the word “rejection” one participant responded, A few weeks ago, I had a meeting with my boss, and my ideas were rejected.” Another said, “My brothers are always talking about going on holiday without me.”
You can see how the second response is vague, it’s generalizing over time, and it’s not a specific event.
Advantages of an over general memory
Researchers at Leuven discovered that students who did poorly on exams and were more specific took longer to recover from the disappointment than those who were more general. The overgeneral students thought less about the details of what happened and so fared better, at least in the short term.
Similarly, overgenerality has been found to be prevalent in Bosnian and Serbian teenagersexposed to the traumas of war. “Some people will discover at a certain stage that being overgeneral is a way of dampening emotional effects,” Dr. Hermans said.
But these researchers say problems can arise when overgenerality becomes an inflexible, blanket style.
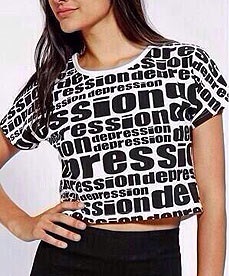
Links to depression
Without detailed memories to draw upon, dispelling a black mood can seem impossible. Patients may remember once having felt happy, but cannot recall specific things that contributed to their happiness, like visiting friends or a favorite restaurant.
“If you’re unhappy and you want to be happy, it’s helpful to have memories that you can navigate through to come up with specific solutions,” Dr. Williams said. “It’s like a safety net.”
What can you do?
Dr. Williams has found that specificity can be increased with training in mindfulness, a form of meditation increasingly popular in combating some types of depression. Subjects are taught to focus on moment-to-moment experiences and to accept their negative thoughts rather than trying to avoid them. It may help by making people more tolerant of negative memories and short-circuit the impulse to escape them, which can lead to over-generality.
Ground to reality – The first thing needs to be grounding to the reality of the present moment. One of the more effective ways to do this is just allowing the feeling in the body to be an anchor to the now. Breathe in, acknowledge the feeling, breathe out, and recognize you are here.
Search for other memories – Ask yourself, are there other memories that speak to an alternative viewpoint. In other words, in respect to the example I gave earlier, are there instances in life where people have paid attention to your needs?
Have compassion – You may just have a natural inclination toward a negative sort of overgeneral memory, so as best you can, be kind to yourself when you notice this happening. This patience and kindness will create a greater sense of resiliency.
Hope for the future
Some experts think such insights could also be helpful in treating depression. For example,Spanish researchers have reported that aging patients showed fewer symptoms of depression and hopelessness after they practiced techniques for retrieving detailed memories.
Exercise your Mind – (taken from mindfulness, a practical guide to finding peace in a frantic world)
Look at the words below. Think of a real event that has happened to you, and that comes into your mind when you see each of these words. Keep in mind or write down what happened. (It doesn’t matter whether the real event happened a long time ago or only recently, but it should be something that lasted for less than one day.)
For example, if ‘fun’ was on of the words, it would be OK to say, ‘I had fun when I went to Jane’s party’, but it would not be OK to say, ‘I always have fun at parties’, because that doesn’t mention a particular event. Do your best to write something for each word.
In each case remember to come up with something that lasted for less than one day.
Think of a time when you felt:
-
Happy
-
Bored
-
Relieved
-
Hopeless
-
Excited
-
Failure
-
Lonely
-
Sad
-
Lucky
-
Relaxed